Restrictive Eating Behaviour
Restrictive Eating Behaviour
Restrictive eating behaviour goes beyond what is commonly termed “fussy eating” or “being picky” with food. Restrictive eating can start in young childhood as displaying a preference for a limited diet. As the child grows up, the repertoire of food choices remain small and may even become narrower in response to a various individual and social experiences.

Meal preparation for a young child with restrictive eating disorder can be challenging for the food preparer. The child may prefer to remain hungry when encouraging them to try new food and offering no suitable replacement. As a parent of that child you can then feel that you are neglecting them and failing to give them nutritious meals. The tension at meal times can increase when the food preparer is enthusiastic about cooking and finds that the time spent on your gastronomic delight does little to inspire the child’s appetite to eat it.
As a disorder, restrictive eating has changed from Selective Eating Disorder (SED) to the group term Avoidant Restrictive Food Intake Disorders (ARFID). It can also be termed as a Food Neophobia.
Do you have restrictive eating problems?
With restrictive eating habits, there is usually a sensory aversion to the unwanted food. The appearance of the food, the colour, the presentation, the taste, the texture, the temperature and/or the smell of the food causes disgust or an anxiety response (panic attack). Seeing the food nearby or talking about the food is enough to provoke the negative response.
Generalised avoidance patterns can usually be identified e.g. the fibrous, crunchy or varying textures found in raw fruit, vegetables or meat; the smooth or lumpy textures found in sauces, or the acidic or spicy tastes found in certain fruits or Asian foods.
But the restrictive eater can also have specific and random aversion issues too, usually caused by an individual direct or indirect bad experience. The bad experience is often forgotten, but it continues to direct the aversion. The problem food appearance, flavour or sensation is then difficult to rationalise; it just looks, tastes or smells horrible, feels unpleasant in the mouth, or is difficult to chew or swallow.
Apathy towards food and mealtimes is a natural consequence of these negative reactions. Pressure to eat can trigger anxiety responses which can then become the focus of the aversion.
Can restrictive eating be connected to other eating disorders and phobias?
Parents of children with restrictive eating patterns may become concerned about their potential anorexia, bulimia or binge eating behaviour. However, a child with restrictive eating disorder does not have the same weight and body image issues connected with these other eating disorders. Instead, the lack of nutrition becomes the concern, threatening to affect the physical development of the growing child, and the future health implications for the adult.
Restrictive eating behaviour, however, can be part of a general neophobia (or fear of anything new) and even connected to OCD (obsessive compulsive disorder). Those with a neophobia feel insecure about trying new things and tend to rigidly stick to their already-formed habits or routines. Avoiding the risk of new food with unknown flavours and textures can be just one aspect of a general neophobia.
The term food phobia is sometimes used to describe restrictive eating behaviour since there are common avoidance patterns and the similar negative emotional responses of fear and disgust. But a food phobic person tends to be preoccupied with contamination and hygiene issues. They worry about the hygienic contents of the food, the way the food is prepared, how it is stored or if it is still safe enough (within its use-by date) to be consumed. They believe that if they eat the food, it will cause a bacteria-related illness or food poisoning (sickness and diarrhoea etc.) If an illness has been associated with a problem food, the food type will then be temporarily or permanently avoided in case of further contamination.
Over-generalisations are common with traumatic experiences. When you connect a “cause” to an illness with symptoms of say, diarrhoea, you can be forgiven for wanting to avoid that “cause” ever again to prevent another bout of diarrhoea. If it’s chicken that did the damage, chicken only needs to be “off” once to be convinced that it will always be “off” in the future.

These illogical and mistaken over-generalised connections can be easily made with “bad” food, however. With food digestion being closely related to your emotional state, anxiety can be the real “cause” of symptoms like diarrhoea and not the food that you happened to eat around the time of experiencing your diarrhoea symptoms. When you believe that food is the culprit, it’s difficult to separate cause and effect. You may just blame the food without realising the impact of your anxiety, because food is an easier object to target. You expect to be unwell, and your anxiety makes you unwell.
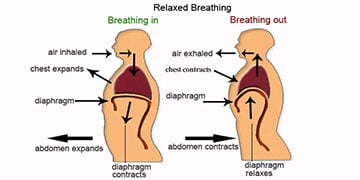
Your anxiety symptoms can also affect other aspects of digestion, not only diarrhoea. When you forcibly eat food that is “bad” or that you dislike, it can cause muscle tension (spasm) in the upper oesophageal tract (and diaphragm). The result of this spasm is difficulty swallowing the food. The body can react by gagging (retching), choking or feeling nauseas (vomiting). In more severe cases it can even cause persistent vomiting (rumination syndrome). Whilst these symptoms are “normal” reactions under the tense conditions triggering them, nobody wants to react in this way. If you persistently react to a particular food by retching, you will naturally want to eliminate that food from your diet.
Restrictive eating and social anxiety
Without parental and family pressure, a young child with restrictive eating behaviour will focus on their own food choices and accept their own boundaries until they are ready to change. But the growing child will inevitably make comparisons with themselves and how others eat. At around the time of teenagehood, the value system typically shifts towards social standards of acceptance. “Fitting in” during social eating occasions has increasing importance and peer judgement gradually leaks into what you should and shouldn’t eat. Just having “different” eating habits might draw attention and embarrassment, which a teenager with restrictive eating behaviour and social anxiety will want to avoid. It could be a high risk situation adversely reacting to new food with everybody watching you. With social anxiety, it’s as if you are constantly on show, but without wanting to give a performance.
School dinners, the increasing number of friend’s parties and formal dining events become a continuous source of anxiety. There is pressure to eat what everyone else is eating in case you stand out. But the anticipation can start days before the event, not knowing what is on the menu, not liking what is on the menu, being in fear of offending the host if you don’t eat everything served on your plate, or feeling guilty about wasting the money of the person buying the set menu food at a fancy restaurant.
It would seem logical and helpful to communicate your restrictive dietary needs, but the inability to assertively communicate your needs is often part of the (social anxiety) dilemma. Just mentioning the issue is likely to bring you attention. It doesn’t matter if you have praise, encouragement or criticism; you just don’t want to be the focus of any attention.
These internal conflicts in being able to handle the situation will build up your anxiety. Your appetite is usually lost by the time the event arrives. Cancelling with notice or not showing up at all increases the guilt of letting people down and losing friends, and acts as a deeper trauma likely to cause the avoidance of all future social dining experiences.
For those who feel under pressure to attend and try new food that you dislike, a panic attack is likely to trigger the digestive muscular spasm symptoms (gagging, choking etc.) described above. It’s distressing enough being at home and provoking these tension-related symptoms. For the socially anxious person who fears embarrassment, displaying these tension-related symptoms at a formal dining occasion like a family wedding, would cause complete humiliation.
Social anxiety then adds another problematic layer to the restrictive eating behaviour. Having a social trauma with that food (or a different food that has similar properties) will associate a deeper avoidance of future social dining experiences.
What causes restrictive eating behaviour?
The causes of restrictive eating behaviour can be linked to physical, emotional/psychological and socio-cultural factors most influential during childhood.
Some developmental disorders and temperamental traits can be inherited from your parents, predisposing you to develop similar patterns of restrictive eating behaviour in childhood. Research by Schreck at Pennsylvania State University found a higher percentage of children with obsessive compulsive disorder and autism are more likely to have selective eating problems.
Children with acute sensory processing abilities (sensory processing disorder) are likely to overreact to “normal” sensory stimuli. The condition causes certain sights, smells, tastes and sensations to overload how their brain handles sensory inputs. Other research suggests that a small percentage of the population are “super tasters”, possessing a gene that heightens their taste response. Super tasters are overwhelmed by certain taste sensations that “non” or “normal” tasters can manage comfortably.

Some children will acquire their selective eating behaviour by imitating parents (or significant authority figures) that also eat a small repertoire of food. Parents can have a selective eating disorder themselves or may be influenced by hectic lifestyle choices. Convenience food like takeaways tends to be high in saturated fat, sugar and salt with many of the ingredients being overcooked. Children can become conditioned to eat only these flavours and textures. This can then set up an expectation for these flavours and textures that are rejected with healthier home cooking food choices. The pressured parent who wants to feed their child quickly (without meal time conflict) will give children what they know that they will eat, rather than spending time extending their curiosity for new food types.
Some (non food-related) learned experiences can be emotionally destructive to the growing child’s eating patterns. Family traumas like parental rowing and abuse can cause constant fear and insecurity. Since appetites are affected by emotions, a child who feels anxious and insecure during meal times may struggle to eat certain flavours and textures. These foods can then be associated with trauma and avoided because they symbolise family trauma.
Other indirect traumas can be caused by seeing a parent or family member choke on a certain type of food. Without an explanation about why the parent has reacted in this way, the young child might identify the food as the cause of this trauma to their parent and avoid it in the future to be safe from danger.
Direct trauma with food is often the major influence of restricted eating behaviour, where the child concludes that the food is associated with the trauma. If the child has a physical or emotional condition (mentioned above) that initially restricts their eating behaviour, then trying food that is outside the “norm” can overwhelm their sensations and prevent them from wanting to eat that food again. If the food causes an illness (food poisoning) or a physical tension-related symptom (when alone or in public), then this food type will again be avoided.
Parents who possess overly strict eating patterns, are controlling and abusive with food will cause lasting damage to a child’s restrictive eating behaviour. The majority of clients who have sought hypnotherapy treatment from me often recall agonising memories of battles with food involving their parents or other significant authority figures. Being force fed certain food, having to stay at the table for hours until the plate is cleared and being punished for not eating the food are common childhood traumas.
The parents may have been subjected to abuse themselves and continue to inflict these abusive and manipulative patterns on their children. Other parents are just overly enthusiastic about their (lack of) “parenting skills” when it comes to eating methods and stimulating a child’s appetite. By forcing the child to eat at just one meal time, they are unaware of the damage that it is doing in the long term. Insisting that the food is “healthy and good for you!” won’t make the food taste or feel any better. Yes, it’s common for some children to avoid the main course when they know that a dessert awaits them, but the child’s manipulation is usually innocent at a young age. It’s up to the parent to tactfully work around this.

Either way, the emotional conflict that these food wars create becomes the association that the child wants to avoid in the future. Eating this food type again as an adult would “bring the horror story back into their lives”. And a child who is defiant then feels that eating this food as an adult would be a victory for the parent because they historically connect “healthy food” with control and manipulation. It’s not surprising that the defiant growing child then opts to stay “unhealthy” to spite the controlling parent.
Treatment for restrictive eating behaviour
Most restrictive eaters would like to broaden their limited food choices. There can be numerous personal and lifestyle changes that can motivate a desire to overcome the restrictive eating behaviour. For example, reaching teenagehood or young adulthood, being in a new relationship and being a new parent are common situations to encourage a dietary change.
Motives to change restrictive eating often include: the limitations it places on your lifestyle, new healthier eating values, feeling embarrassed about how the restrictive eating appears in public and how the restrictive diet is affecting significant others e.g. your partner or your children. A successful treatment will confront the variety of issues that cause your food aversion and identify progressive realistic and achievable goals.
A combination of cognitive behavioural therapy and systematic desensitisation are conventional approaches used to treat restrictive eating behaviour. The strategies will vary for adults and children. The teenager or adult who chooses to start therapy will arrive with a motive for change. Young children are still responsive to the conditioning patterns offered by their parents. Both the young children and parents will discuss the child’s current restrictive eating behaviour and how it is conditioned by the parents. A treatment plan is discussed and new conditioning strategies can be suggested. For example, the emphasis with young children can focus on offering non-food related rewards (e.g. a sticker) for being curious about tasting food that is new or disliked. It’s important to avoid giving food-related rewards like sweets. The experience should be fun with the parents similarly being involved in the new taster sessions.
Exposure to the new food needs to be repetitive (with trials completed at least once a day) and thus keeping a stock of that food item is essential for continuity. It can take ten attempts with the new food to convert it from a “dislike” to “acceptance”. A parent typically surrenders to a child’s refusal after two attempts and will then give the child what they know they will eat. This prevents “failure” on both parts and reduces food wastage, but the submission is premature for long term gains. When persevering with the food trials, the food doesn’t have to be “loved”, more that the anxiety and tension-related symptoms are alleviated. The new food item can then be “accepted” and can be included into the general meal.
Some parents try to disguise food to reduce the anticipation of rejection. This can have the benefit of minimising strong flavours or rough textures when they are liquidised into a soup for example. The child has already eaten the food that they “dislike” (albeit in a disguised form) and this can be used as a reference to reduce the fearful reaction when they say “I don’t like carrots!” The parent then (smugly) replies “you didn’t object to the carrots in my homemade soup that you’ve been eating on the last ten occasions!” If applied carefully, it can enable the child to separate the “danger” that a disliked food might cause them. There is a risk however. When outsmarting the child too frequently or too obviously (when the carrot isn’t disguised enough), the child can feel betrayed and will distrust not only the parent’s future cooking, but other’s attempts to control what they want to eat. It’s far better to gain their approval with trials, praising being curious with new food and ignoring their refusal of a food. Criticising the refusal will hinder their progress.

Another useful way to encourage children’s curiosity with food is to involve them in the preparation, cooking and serving of food. This can still be done with some of the food that they dislike e.g. using a selection of liked and disliked food to top a pizza. This helps children be creative with food, learn about textures, and how food changes in flavour and appearance when it is being cooked. Again, they should not be forced to eat the disliked food, more that they gradually get used to it being present. When they are involved in family meal preparation, it gives them a sense of responsibility and ownership with the food that can transfer into curiosity and acceptance in the long term.
How can hypnotherapy help restrictive eating behaviour?
My hypnotherapy treatment for selective eating behaviour incorporates cognitive behavioural therapy approach to challenge negative attitudes and systematic desensitisation to encourage graduated exposure to disliked foods.
Hypnotherapy is used to reduce anticipatory anxiety and control the anxiety reactions when sampling the food. Positive visualisation of food eaten can accelerate the food trials, acting as pleasurable experiences that have already been practised in reality. Regression is also used to remove past negative “causes” of an aversion, releasing the beliefs that are contributing to an emotional block with disliked food.